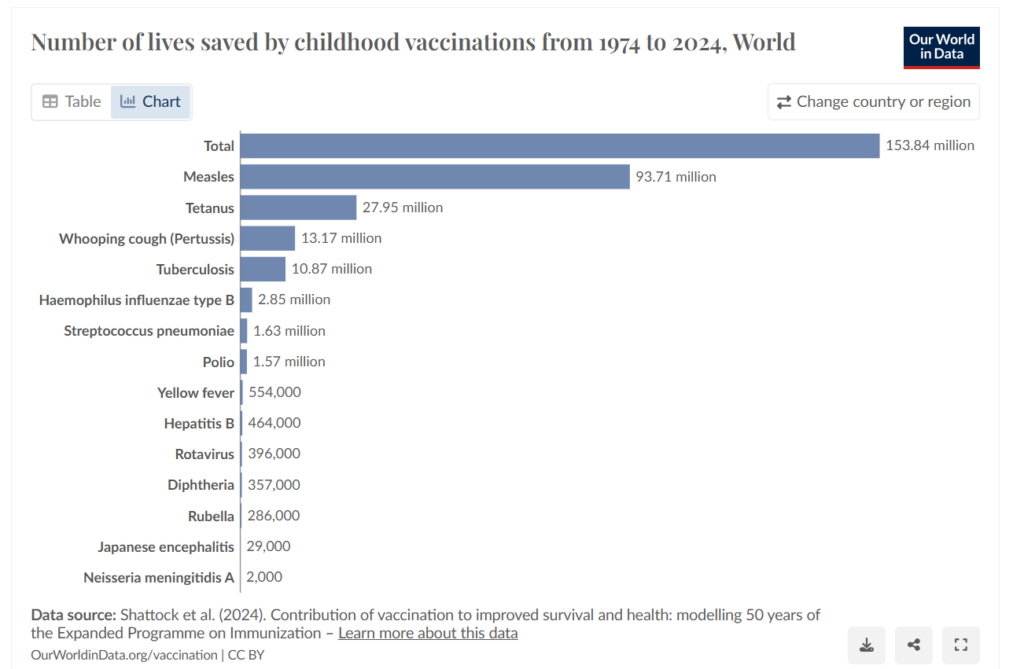
Recently someone complained to me online that he could never consider Christianity because computer modelling had shown that without the Church’s interference, science would be 400 years further advanced than it is.
There is no evidence of any computer modelling claiming that science would be 400 years more advanced without Church suppression. This assertion stems from debunked claims propagated in 19th-century “conflict thesis” books like John Draper’s History of the Conflict between Religion and Science (1874), often visualized in misleading graphs showing stalled progress during the Middle Ages. Such graphs claiming massive delays of 400–1,000 years circulate online but have been labelled “complete bulls*#t” by historians.
Even if such computer modelling had been conducted, it could tell us nothing new. Computer models cannot produce new information. They can only give back what is input, sometimes presenting information in new ways. They reflect the information and assumptions put into them.
The only objective way a delay caused by Christianity could be measured would be to compare the development of science in the West with the development of science in other societies. But this cannot be done, for the simple reason that the Christian West is the only place where the scientific method, and science itself; the careful, systematic, objective study of material reality for its own sake, ever developed.

But how can this be, if Christianity is the great oppressor of science? There are two answers to this question. First, Judeo-Christian metaphysics are a necessary foundation for science. And secondly, far from being an oppressor of objective study and truth-seeking, the Church has always been the great supporter and defender of science. I will explain each of these claims in turn.
I am not the first to notice that science arose only where Christianity was the common faith. For example:
“The fundamental paradigm of science; its invariable stillbirths in all ancient cultures and its only viable birth in a Europe which Christian faith in the Creator had helped to form.” Stanley L. Jaki, Theologian and physicist, The Road of Science and the Ways to God.
“Theological assumptions unique to Christianity explain why science was born only in Christian Europe. Contrary to the received wisdom, religion and science not only were compatible; they were inseparable.” Rodney Stark, Historian, For the Glory of God.
But why? What are these theological and metaphysical assumptions that are unique to the West, and underpin the development of science?
Science and the scientific method could only take hold in a world view that:
- The material world is objectively real, not simply an illusion; why would you bother to investigate something that wasn’t real?
- The material world is good – something worth investigating, not an evil to be escaped from
- That the material world is ordered according to rules which can be investigated and understood, and not by the whim of inhabiting spirits or an god who rules by fiat
- And finally, that faith has nothing to fear from the truth.
This is the standard Western understanding of reality, so it seems difficult to many Westerners to imagine that people could think otherwise. But in reality this combination of beliefs is uniquely Judeo-Christian. This is why science, the systematic and objective study of reality for its own sake, has taken root and flourished in the West as nowhere else, which has in turn given the West enormous advances and advantages in science and technology.
The usual response to this claim by detractors is: “But what about Galileo?” The fact that most people can think of only one possible counter-example in 2,000 years of Church history is itself telling. In reality, Galileo was never tortured, never imprisoned, and was always free to teach the Copernican theory as a theory, as had been done in other Catholic universities throughout Europe since heliocentric theory was first proposed by Nicholas Copernicus, a Catholic priest. When talking about this period in history, “Catholic universities” is a tautology. By the year 1500 there about 100 universities in Europe; every one of them was Catholic.
The issue with Galileo was that the Church insisted students be taught every reasonable alternative, with the evidence for and against, and allowed to make up their own minds. Galileo refused to teach anything except his own pet theories. In many of these, he was completely wrong. For example, as Einstein noted in 1953, Galileo’s theories about tidal action were nonsense. Galileo believed the rings of Saturn were not rings but a large moon on either side. He was savage in his attacks on Jesuit astronomer Orazio Grazzi, who correctly described comets as small heavenly bodies, while Galileo insisted they were reflections shining on vapours rising from the earth. In each of these instances, Galileo refused to teach or consider any other possibility.
As philosopher of science and Berkeley professor Paul Feyerabend noted, it was the Church, not Galileo, which was on the side of reason and science: “The Church at the time of Galileo was much more faithful to reason than Galileo himself, and… her verdict against Galileo was rational and just.” Paul Feyerabend (from Against Method, 1975).
Add to this that Catholic priests were founders of several branches of science. Marin Mersenne (1588-1648), a priest of the Minimite order, founded the science of acoustics (the physics of sound), and advanced music theory and knowledge of prime numbers. The science of geology started with the work of Bl. Nicolas Steno (1638-1686), who discovered the origin of sedimentary rock and fossils and established the laws of stratigraphy. One of the founders of astrophysics was the Jesuit priest Angelo Secchi (1818-1878), who pioneered the use of spectroscopy to study stars and developed the first systematic classification of them. The Augustinian friar Gregor Mendel (1822-1884) is regarded as “the father of genetics.” The Big Bang theory was first proposed by Fr. Georges Lemaître (1894-1966), a Belgian priest and theoretical physicist.
These are only a tiny proportion of the total number of Catholic scientists who have made major contributions. There is a list on Wikipedia, which, impressive as it is, includes only lay people. https://en.wikipedia.org/wiki/List_of_lay_Catholic_scientists A list of clergy, including those I mentioned above, would be just as long.
In the late 1700s, one quarter of all the astronomical observatories in the world were run by the Jesuit order, as is the Vatican Observatory to this day. The Jesuits were also pioneers in the field of seismology, their far-flung missionaries setting up seismological stations around the globe.
It is worth noting that the medieval Church held natural science (then called “natural philosophy”) in such high esteem that it was a prerequisite for studying theology in medieval universities.
The Church’s insistence that students be presented with the evidence for and against all reasonable theories on any issue, required to do their own research, encouraged to make up their minds on the basis of the evidence, and then calmly and rationally argue their point of view with their professors and other students, is still the key to effective learning, in opposition to agenda driven lecturing.
Now, as for the last 2,000 years, the Church remains the patron and defender of science.