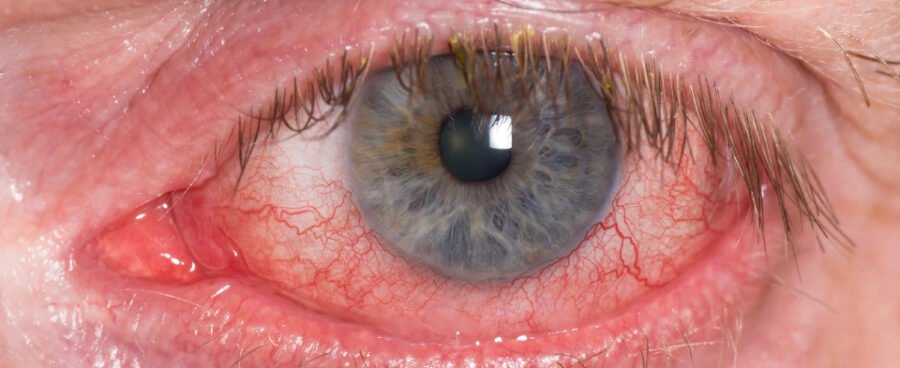
On May 12th an article appeared in News Ltd press and digital outlets relating the story of a young man who was diagnosed with Retinal Vein Occlusion a few days after receiving his second dose of the Moderna COVID vaccine.
Cody Hose-Ross, who is a twenty-one year old tradesman, applied for compensation under the Government’s vaccine injury compensation scheme. An eye surgeon, Dr Peter Davies, supported his claim, writing “His colour photography shows an unusual discolouration in the temporal retina of the right eye which is not seen in the left eye and my interpretation is that it represents area where the vaccine has directly landed in the retinal circulation leading to patchy ischaemia of the outer retinal layers in the deep capillary plexus.”
The vaccine “landed directly in the retinal circulation.” Right.
Dr Davies’s opinions were supported by Professor Peter McCluskey, also an eye surgeon. Essentially, and apart from vaccine “landing directly in the retinal circulation” a claim so ridiculous it belongs in Mad Magazine, the argument by both experts was that Hose-Ross’s RVO appeared soon after his second dose of vaccine, so was probably caused by it.
Is that reasonable? Is RVO so rare that doctors and compensation bodies can be sure that any incidence after vaccination was caused by the vaccination?
It is important that compensation courts and assessment bodies be on the generous side of fair. People who have suffered one of the tiny number of genuine serious vaccine injuries should be given every support they need. It is also important that those courts and other bodies be truthful. Injuries or events that are not a consequence of vaccination should not receive compensation.
People commonly and naturally attribute adverse events after vaccination to the vaccination. In the large Pfizer COVID-19 vaccine trials 1% of those who received the vaccine reported a significant adverse effect; something more than headache, mild fever or soreness at the site. But 1.7% of those who received the placebo also reported serious adverse effects. Obviously, none of those effects could have been caused by the vaccine – those people had not received the vaccine. But then how many of the effects reported by the 1% of people in the vaccine group were caused by the vaccine? How would we know?
Something that needs to be kept in mind all the time when considering whether an event was a direct consequence of another event is this: just because something happens after another something, does not mean the first something caused the second. For example, imagine you change the brand of coffee you drink. The very first morning you use the new coffee, you get a flat tyre on the way to work. Did the coffee cause the flat tyre? How do you know? Most people would answer no, because even though getting a flat tyre is rare, it does happen, and also there is no obvious way a change in coffee could cause a flat tyre.
The same considerations apply in medicine. First, if x is supposed to have caused y, is there is a clear correlation between x and y? And second, is there a mechanism by which x could cause y?
How does this relate to COVID vaccines and RVO?
A study conducted in Australia in 2006 in persons forty-nine years of age and older found that the cumulative ten year incidence rate for Retinal Vein Occlusion was 1.6%. This means an averaged rate of 0.16% per year or approximately 1600 people per year per million diagnosed with RVO. Increasing age is correlated with higher rates of RVO, as is high blood pressure, so the rate for the general population may be lower.
To account for this, let’s say an actual average of half this rate; eight hundred people diagnosed with RVO each year in Australia. This matches with recorded incidence figures in Australia and around the world.
This means about sixty-seven people diagnosed with RVO every month in Australia. Important to note is that this rate has not changed since COVID-19 vaccines were introduced.
Over the last two years, most Australians have had three doses of a COVID-19 vaccine. One every eight months. What this means is that on average, every month, just over eight people in Australia will be diagnosed with RVO within thirty days of having received a COVID vaccine.
Just to make that clear, what happens anyway, vaccine or not, is that on average, every month, just over eight people in Australia will be diagnosed with RVO within thirty days of receiving a COVID vaccine.
The question is not “Did some people get RVO after having a vaccine?” Of course they did and will, just as some people will over-boil their eggs, have car accidents, get a bonus at work, get married.. None of these things is related to vaccination status. The question is “Are people who have been vaccinated getting RVO at a higher rate than those who have not?”
Over the last couple of weeks somewhat distorted interpretations of a recent paper have been passed around social media by antivax activists. They claim this paper was published in Nature. It was actually published in NPJ Vaccines. NPJ Vaccines is part of the Nature family, but it is not Nature. This matters because accuracy matters.
The finding of this paper was not that a link between COVID vaccination and increased onset of RVO was proven, but that “Retinal vascular occlusion may not be a coincidental finding after COVID-19 vaccination.” This is a very long way from a proven connection.
Another, larger study was published in JAMA Ophthalmology only a month before. This study, which considered some of the same data as the NPJ paper, found “No evidence suggesting an association between the mRNA COVID-19 vaccination and newly diagnosed RVO.”
The best interpretation of these two papers and other evidence at this stage is that even with careful analysis of a sample size of over three million patients, there is insufficient basis to claim a connection between COVID-19 vaccination and the onset of RVO.



Leave a Reply